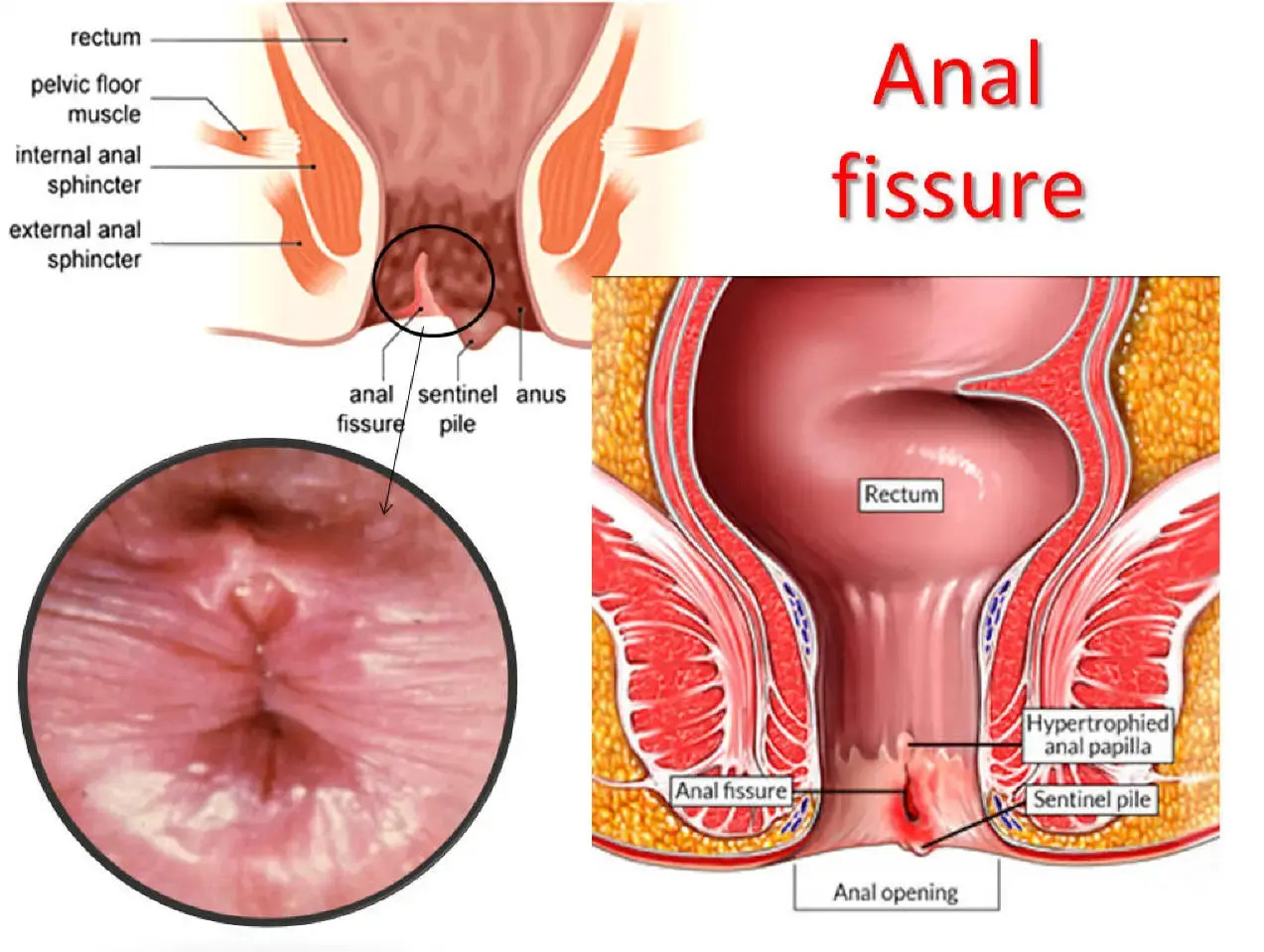
An anal fissure is a small tear or crack in the thin, moist tissue (mucosa) that lines the anus. This tear typically occurs in the posterior midline of the anal canal, though it can sometimes be located elsewhere. Think of it like a paper cut in a very sensitive area.
Causes of Anal Fissures
The primary cause of an anal fissure is trauma to the anal canal, most often due to the passage of a hard or large stool. However, several factors can contribute to their development:
- Constipation: Straining during bowel movements and passing hard, dry stools is the most common culprit.
- Diarrhea: Frequent bowel movements, especially if they are forceful, can also irritate and tear the anal lining.
- Childbirth: The strain and pressure during delivery can sometimes lead to anal fissures in women.
- Crohn's Disease or other inflammatory bowel diseases: These conditions can make the anal tissue more fragile and prone to tearing.
- Reduced blood flow: The posterior midline of the anus naturally has less blood flow, which can hinder healing and make it more susceptible to fissures.
- Anal intercourse: Can occasionally cause trauma leading to a fissure.
Symptoms of an Anal Fissure
The symptoms of an anal fissure can range from mild discomfort to severe pain, and they often include:
- Sharp pain during bowel movements: This is the hallmark symptom, often described as a tearing, burning, or knife-like sensation.
- Pain after bowel movements: The pain can persist for minutes to several hours after passing stool.
- Bright red blood on the stool or toilet paper: This usually appears as streaks of blood.
- A visible crack in the skin around the anus.
- A small lump or skin tag near the fissure (sentinel pile): This is often a sign of a chronic fissure.
- Itching or irritation around the anus.
Diagnosis
A doctor can usually diagnose an anal fissure by reviewing your symptoms and performing a gentle physical examination. This may involve a visual inspection of the anal area. In some cases, a digital rectal exam or an anoscopy might be performed, but often these are avoided if the pain is severe, to prevent further discomfort.
Treatment Options
The good news is that most acute anal fissures (those that have been present for less than 6-8 weeks) heal with conservative, non-surgical treatments. Chronic fissures, however, may require more advanced interventions.
Conservative Treatments (First-line)
Dietary Changes:
- Increase Fiber Intake: Eating a diet rich in fiber (fruits, vegetables, whole grains) helps soften stools. Aim for 25-35 grams of fiber per day.
- Stay Hydrated: Drinking plenty of water helps keep stools soft and easier to pass.
- Stool Softeners: Over-the-counter stool softeners can help prevent straining.
- Sitz Baths: Soaking the anal area in warm water for 15-20 minutes, 2-3 times a day, can help relax the anal sphincter, reduce pain, and promote blood flow for healing.
Topical Medications:
- Nitroglycerin Ointment: This helps relax the anal sphincter by increasing blood flow to the area, aiding healing.
- Calcium Channel Blocker Ointments (e.g., Nifedipine, Diltiazem): These also work by relaxing the sphincter muscles.
- Lidocaine Cream: A topical anesthetic to numb the area and relieve pain.
Other Treatments for Chronic Fissures
If conservative treatments are unsuccessful, especially for chronic fissures, other options may be considered:
- Botulinum Toxin (Botox) Injection: A small amount of Botox can be injected into the internal anal sphincter to temporarily paralyze it, reducing spasm and allowing the fissure to heal. This effect typically lasts for several months.
- Surgery (Lateral Internal Sphincterotomy - LIS): This is considered the most effective treatment for chronic fissures. During LIS, a small portion of the internal anal sphincter muscle is cut. This permanently reduces sphincter pressure, allowing the fissure to heal. While highly effective, it carries a small risk of incontinence.
- Fissurectomy with or without advancement flap: This involves surgically removing the fissure and covering the defect with healthy tissue.
Preventing Recurrence
Once a fissure has healed, preventing its recurrence is crucial. This involves maintaining soft stools through a high-fiber diet and adequate hydration, avoiding straining during bowel movements, and addressing any underlying conditions like constipation or diarrhea.
When to See a Doctor
If you experience persistent anal pain, bleeding, or suspect you have an anal fissure, it's important to see a doctor. While often benign, these symptoms can sometimes indicate other more serious conditions. A healthcare professional can provide an accurate diagnosis and recommend the most appropriate treatment plan for you.